Free Do Not Resuscitate Order Form
A Do Not Resuscitate Order (DNR) is a legal document that allows individuals to refuse resuscitation efforts in the event of cardiac or respiratory arrest. This form reflects a person's wishes regarding end-of-life care, ensuring that medical professionals honor their decisions. Understanding the implications of a DNR can help individuals make informed choices about their healthcare preferences.
Open Do Not Resuscitate Order Editor Now
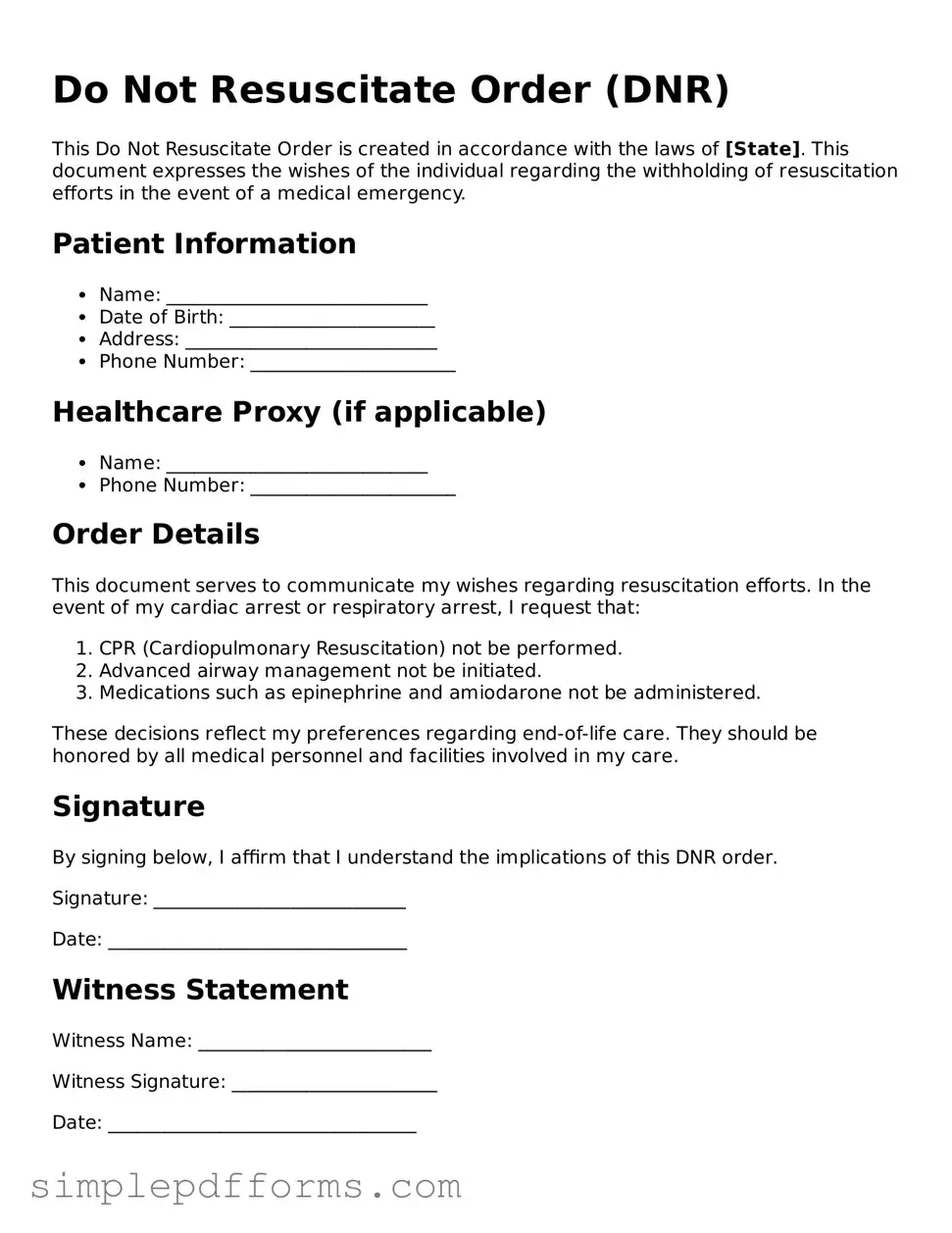
Free Do Not Resuscitate Order Form
Open Do Not Resuscitate Order Editor Now
Open Do Not Resuscitate Order Editor Now
or
Get Do Not Resuscitate Order PDF Form
Your form is waiting for completion
Complete Do Not Resuscitate Order online in minutes with ease.