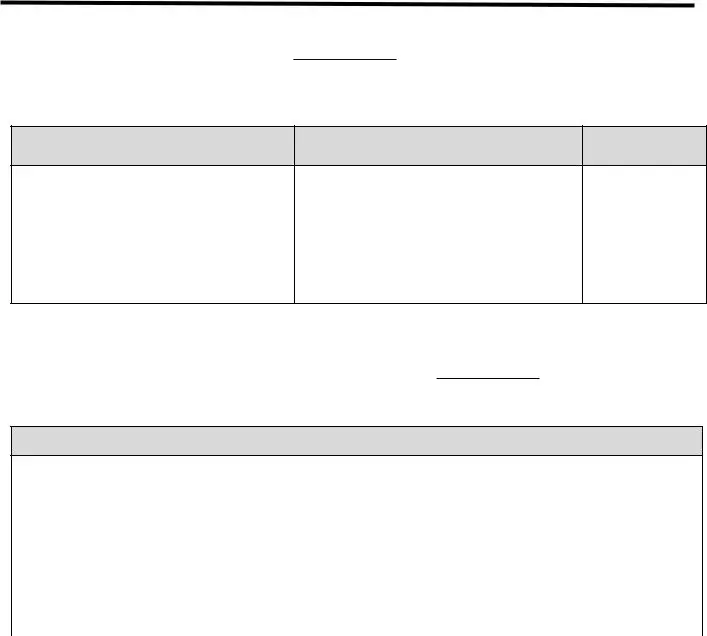
Fill a Valid Advance Beneficiary Notice of Non-coverage Form
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document that informs Medicare beneficiaries when a service or item may not be covered by Medicare. This notice allows patients to make informed decisions about their healthcare and potential costs. Understanding the ABN can help avoid unexpected medical bills and ensure that beneficiaries are aware of their options.
Open Advance Beneficiary Notice of Non-coverage Editor Now
Fill a Valid Advance Beneficiary Notice of Non-coverage Form
Open Advance Beneficiary Notice of Non-coverage Editor Now
Open Advance Beneficiary Notice of Non-coverage Editor Now
or
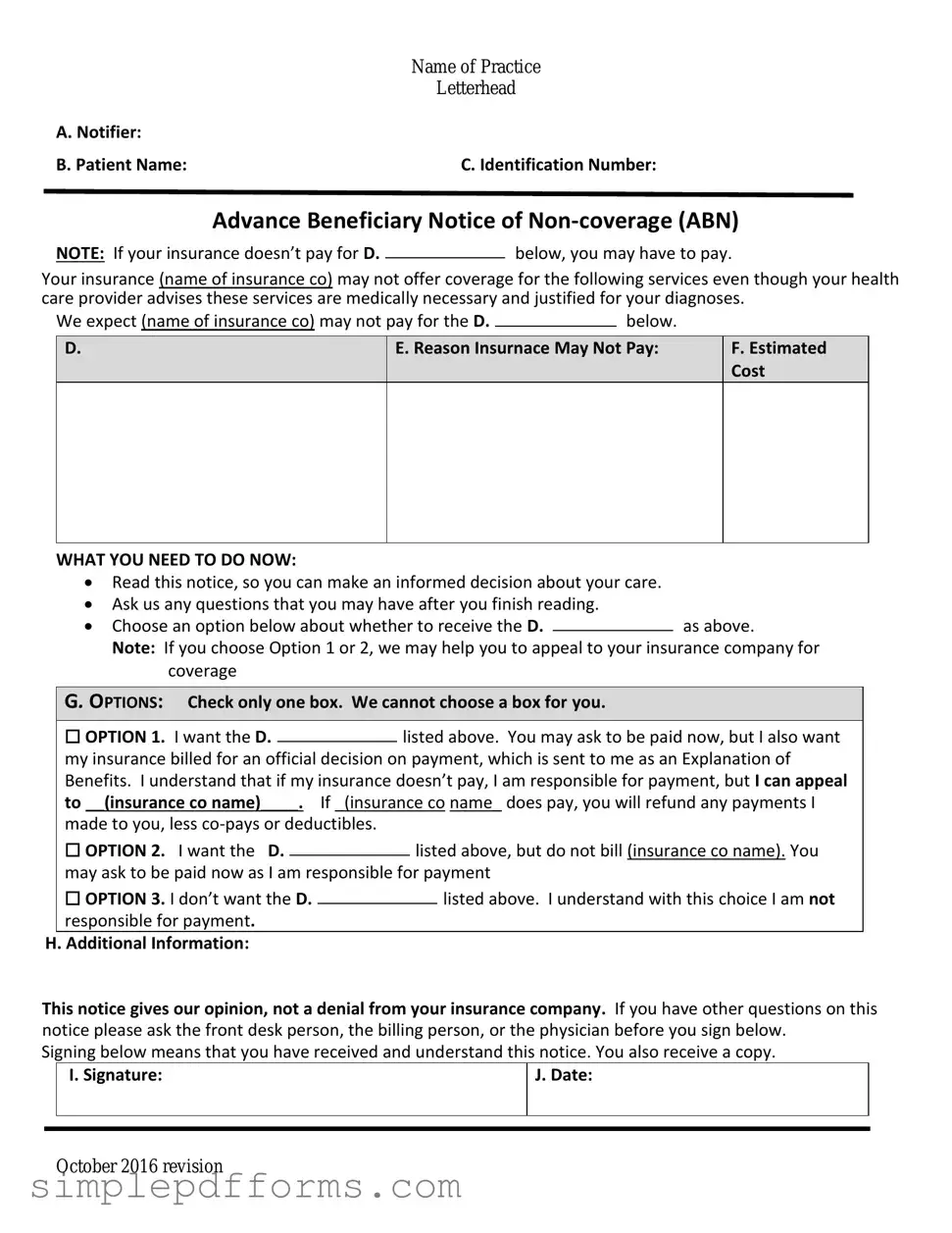
Get Advance Beneficiary Notice of Non-coverage PDF Form
Your form is waiting for completion
Complete Advance Beneficiary Notice of Non-coverage online in minutes with ease.